Frostbite
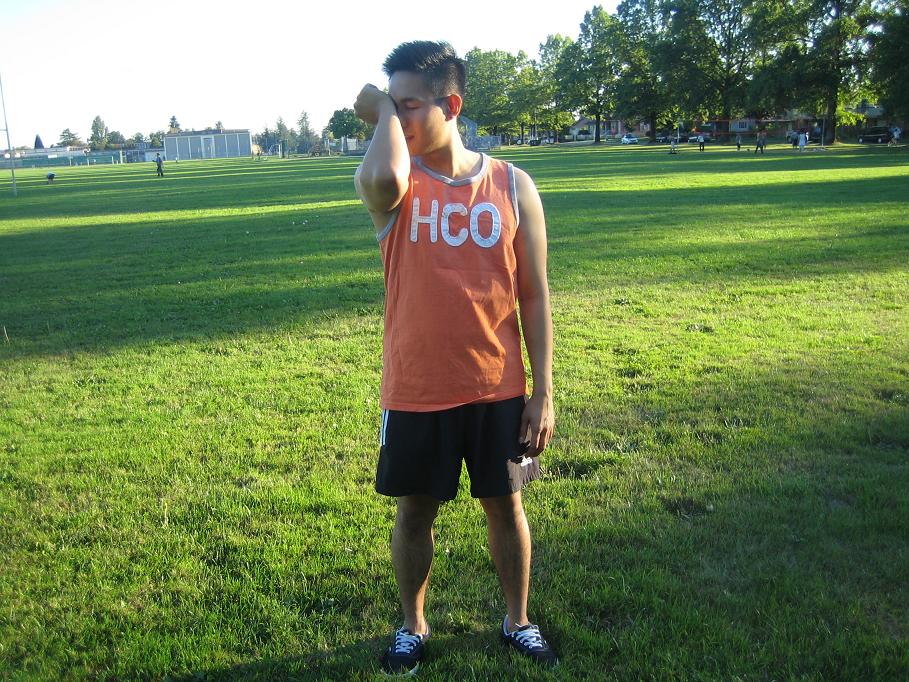
A frostbite is an injury caused by prolonged exposure to cold temperatures, this kind of injury freezes the skin and its underlying layers. Frostbite can lead to serious issues and may cause a limb to cease functioning and lead to gangrene which requires amputation. Frostbite commonly occurs on extremities such as your fingers, toes, nose, […]